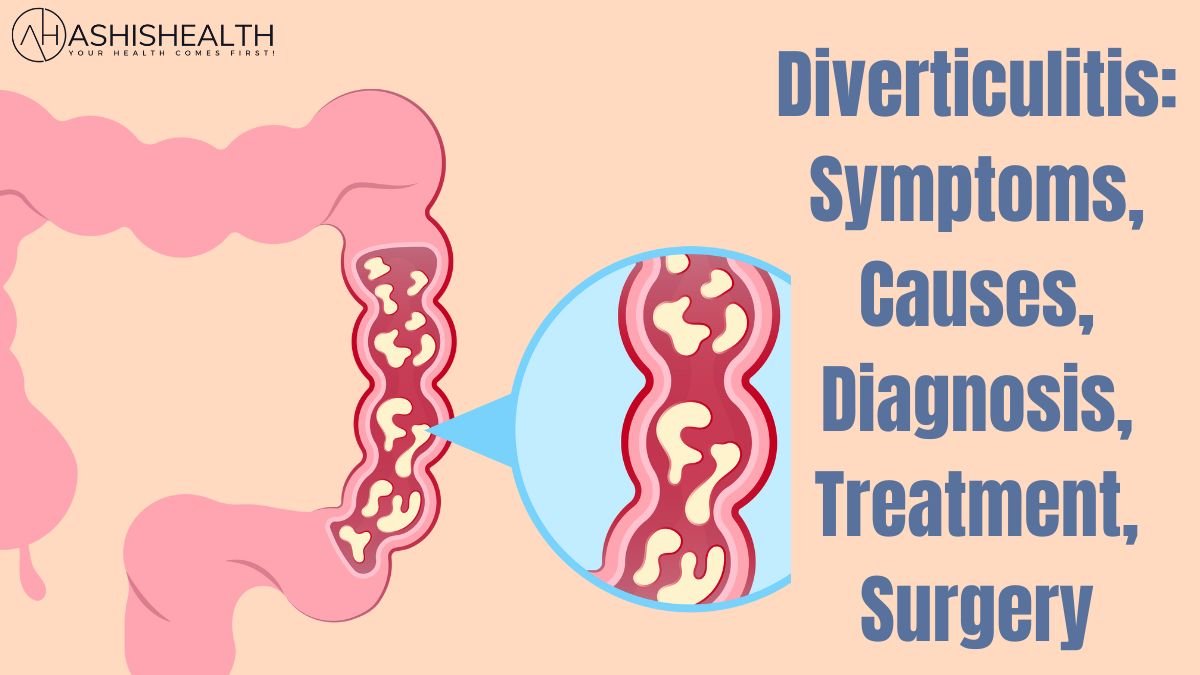
Diverticulitis is a common ailment that develops when the diverticula, or small, expanding pouches, in the colon’s lining become infected or inflamed. It precise origin is unknown, however, it appears to be associated with a low-fiber diet, which can promote constipation and increased colon pressure. Diverticulitis can cause symptoms such as stomach pain, fever, nausea, and changes in bowel patterns. A course of antibiotics and a brief transition to a low-fiber diet are frequently used as treatments to help the colon heal. Hospitalization and surgery may be required in more serious situations.
What Are the Symptoms of Diverticulitis?

It is a common condition that occurs when small, bulging pouches (diverticula) in the lining of the colon become inflamed or infected. The exact cause of diverticulitis is not entirely clear, but it is believed to be related to a low-fiber diet, which can lead to constipation and increased pressure in the colon. Symptoms of diverticulitis can include abdominal pain, fever, nausea, and changes in bowel habits. Treatment typically involves a course of antibiotics and a temporary switch to a low-fiber diet to allow the colon to heal. In more severe cases, hospitalization and surgery may be necessary.
What Causes Diverticulitis?

Diverticulitis is a disorder that develops when the small, protruding pouches or sacs, known as diverticula, that form in the lining of the digestive tract, become inflamed or infected. It is believed to be the result of a number of factors, including a low-fiber diet, aging, obesity, smoking, inactivity, and genetics. The actual cause of diverticulitis is unknown. Diverticula may develop in the colon if it lacks fiber, which might cause it to weaken.
What are the Complications of Diverticulitis?
Abscesses, or pus-filled pockets, are a frequent consequence that can appear in the infected diverticula or in adjacent tissue. Colon perforation is a risky side effect that can happen when infection and inflammation damage the colon’s wall and cause it to break. This may cause an infection to spread to the abdominal cavity, which could be fatal.
How is Diverticulitis Diagnosed?
Doctors often do a physical examination, record a patient’s medical history, and order testing to identify diverticulitis. The doctor will press on the abdomen during the physical examination to feel for any soreness, pain, or inflammation. The patient’s symptoms, medical background, and any drugs they may be taking will all be better understood by the doctor thanks to the medical history. Blood tests may also be required to look for indicators of illness or irritation.
How is Diverticulitis Treated?
Diverticulitis is often treated with an antibiotic cocktail and dietary modifications. It’s critical to stay away from foods that can aggravate the colon, like spicy or high-fiber foods, and to consume a low-fiber diet up until symptoms subside. Hospitalization and intravenous antibiotics may be required in more severe diverticulitis patients. In some uncommon situations, surgery may also be advised, especially if there is a chance of complications or recurrence.
Diet and diverticulitis

Diverticulitis management can benefit greatly from dietary changes. In order to give the digestive tract time to relax and recover during an acute bout of diverticulitis, a low-fiber diet may be advised. White bread, processed cereals, spaghetti, and canned fruits and vegetables are a few examples of such items. Avoid eating foods high in fiber, such as whole grains, fruits, and vegetables.
Dietary Changes

It is advised to eat a high-fiber diet since it can soften and bulk up feces, making them easier to pass and relieving strain on the colon. Fruits and vegetables, whole grains, legumes, and veggies are excellent sources of fiber. Constipation can be avoided by drinking plenty of fluids. Avoiding spicy or fatty foods is advised because they may make symptoms worse.
Medication

The severity of the ailment, along with other elements including the patient’s age and medical history, will all play a role in the precise drug that is prescribed. Ciprofloxacin and metronidazole are the most often used antibiotics to treat diverticulitis. Usually, oral administration of these drugs lasts for seven to ten days.
Surgery for Diverticulitis
Diverticulitis surgery is frequently determined by the patient’s general health, the intensity and frequency of the attacks, and the diverticulitis itself. Surgery might be advised if Diverticulitis bouts have occurred on numerous occasions for the patient, and none of them have improved with medication. Abscess, perforation, or fistula are only a few of the patient’s difficulties. Colon obstruction affects the sufferer.
Home Remedies for Diverticulitis
It can typically be treated medically, but there are some at-home therapies that may help reduce symptoms and stop flare-ups. By consuming more fruits, vegetables, and whole grains, one of the most effective treatments is to boost fiber intake. Constipation, which can increase symptoms, can be avoided and can help regulate bowel motions. Additionally, you may lessen inflammation and improve your overall digestive health by drinking plenty of water, exercising frequently, and managing your stress.
Meckel’s Diverticulitis
A pouch or sac protrudes from the small intestinal wall in Meckel’s diverticulum, a congenital malformation. It is a piece of the yolk sac-to-developing fetus’s connection to the embryonic vitelline duct. Meckel’s diverticulum usually causes no symptoms and is risk-free. The condition known as Meckel’s diverticulitis, however, can occur in some instances when it becomes inflamed and infected.
Preventing Diverticulitis
Diverticulitis can be avoided by consuming a high-fiber diet, staying hydrated, and engaging in regular exercise that encourages bowel regularity. Consuming foods high in fiber, such as fruits, vegetables, whole grains, and legumes, can help prevent constipation and lessen the strain on the intestinal walls, which lowers the risk of developing diverticula.
Risk factors for Diverticulitis
Diverticulitis is more likely to occur as a result of a number of risk factors. The majority of cases affect adults over 50, making age a crucial determinant. A diet deficient in fiber can also cause diverticulitis since it can cause constipation and raise intestinal pressure. Obesity, smoking, inactivity, and some medications, like nonsteroidal anti-inflammatory drugs (NSAIDs), are additional risk factors.
Diverticulitis vs. Diverticulosis

Two disorders that affect the colon (large intestine) are diverticulitis and diverticular disease. Small, protruding pouches (diverticula) develop in the colon’s lining as a result of the disorder known as diverticulosis. It is a prevalent disorder that frequently goes undiagnosed, especially in elderly persons. Diverticulitis is a condition in which one or more diverticula swell up or become infected. It can cause symptoms such as nausea, vomiting, diarrhea, constipation, and abdominal pain.
FAQs
What is the Main Cause of Diverticulitis?
Diverticula are hypothesized to occur mostly as a result of a low-fiber diet and genetic susceptibility. The colon has to work harder to pass waste through the digestive tract when the diet is poor in fiber. The colon wall’s weak regions may protrude and develop pouches (diverticula) as a result of the increased pressure.
Is Diverticulitis very Serious?
It has the potential to be a dangerous ailment, but the degree of the condition’s seriousness will depend on how much inflammation or infection is there and how long it has been there.
What is the best treatment for Diverticulosis?
Diverticulosis responds best to dietary adjustments and increased physical activity. Including fruits, vegetables, and whole grains in a high-fiber diet can assist to soften stool and reduce constipation, which relieves strain on the colon. It’s also crucial to drink enough water. Doctors may advise laxatives or fiber supplements.
Also Read: Endometriosis: Causes, Complications, and Treatment